Volumetric Capnography
The measurement of the CO2 signal in time is very useful for the detection of several conditions both during the anesthesia and outside the operating room (especially in the intensive care unit). Among the most frequent applications there are: confirmation of endotracheal intubation, monitoring of alveolar ventilation during surgery and early detection of the possibility of disconnection of the patient from the ventilator.
During the last few years several new applications have been developed: monitoring of hypoventilation during sedation in spontaneous ventilation, evaluation of respiratory mechanics (MV), evaluation of the effectiveness of cardiopulmonary resuscitation, assistance during the percutaneous tracheostomy process, confirmation of the response of the nervous system during apnea, and even reduce costs and interventions associated to blood gases analysis and metabolic rate.
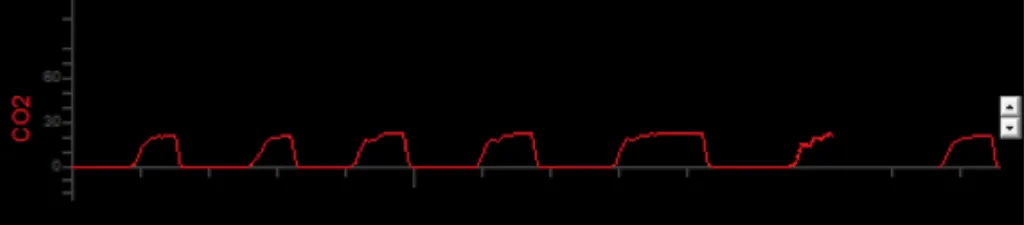
By synchronizing the the volume signal with CO2 signal, much richer information can be obtained. Putting together the parametric CO2 graph vs. the exhaled volume, the Volumetric Capnography graph is constructed.
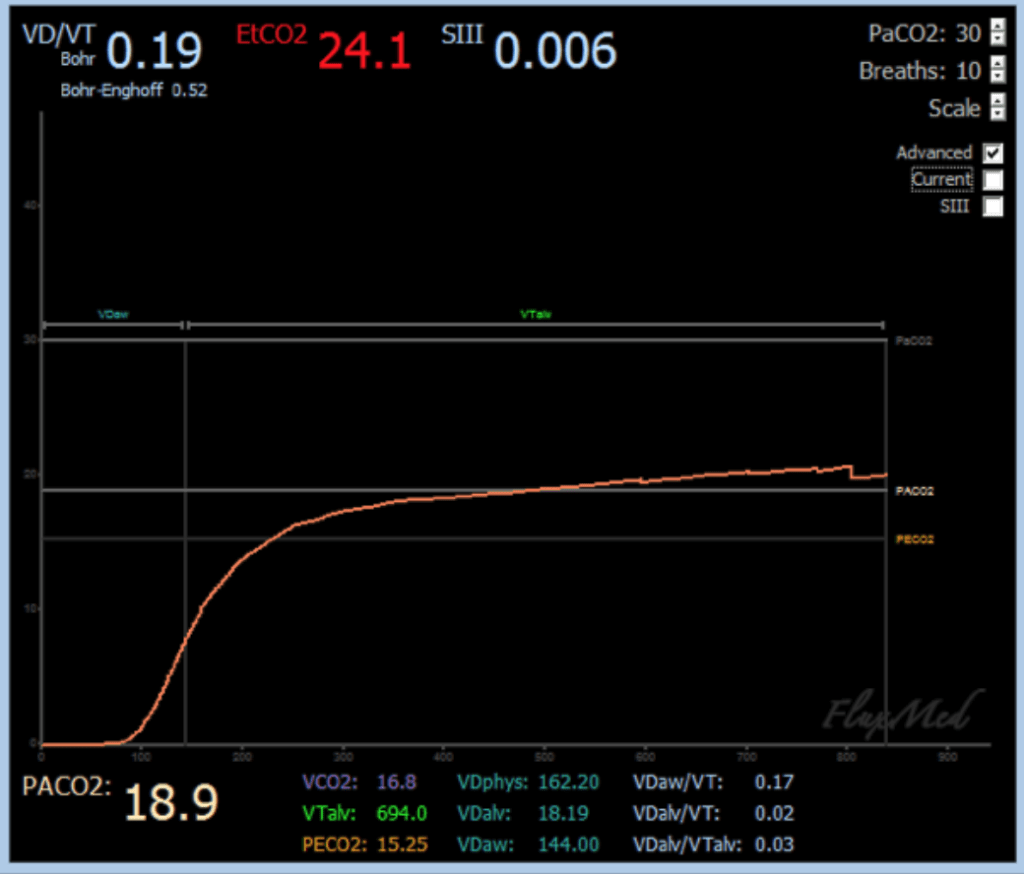
From a clinical point of view, very valuable information can be obtained since it allows calculating alveolar dead space and cardiac output. The monitoring of the alveolar dead space can be very useful to evaluate the response to recruitment maneuvers and the pathophysiology of the patient's disease (especially in ARDS and in the diagnosis of pulmonary thromboembolism).
The monitoring of the dead space, with different configurations of the respirator allows better understanding of the ventilation, perfusion and metabolic characteristics of the patient.
The production of CO2 (VCO2) is the area under the curve. The expired fraction of CO2 (PECO2) is the average expired value. A new algorithm makes it possible to calculate the alveolar CO2 concentration (PACO2). Using the Bohr equation, the physiological dead space (Vd / Vt) and its components can be calculated. All this is done breath-by-breath and non-invasively.
If the patient is taken a sample of arterial gases in order to measure arterial concentration of CO2 (PaCO2), using the Bohr-Enghoff equation, the patient's shunt can be estimated.
The FluxView software automatically calculates all the following parameters through an easy and user-friendly user interface.
| Parameters | Description |
|---|---|
| VD/Vt Bohr | Ratio of physiological dead space and tidal volume calculated with the Bohr equation |
| VD/Vt Bohr-Enghoff | Ratio of physiological dead space and tidal volume calculated with the Bohr equation |
| EtCO2 | Concentration of CO2 at the end of expiration |
| SIII | Slope Phase III |
| PACO2 | Alveolar CO2 partial pressure |
| VCO2 | Volume of CO2 produced by respiration |
| VTalv | Alveolar current volume |
| PECO2 | Expired fraction of CO2 |
| VDphys | Physiological dead space |
| VDalv | Alveolar dead space |
| VDaw | Dead space of the airway |
| VDaw/VT | Relationship of the dead space of the airway and the tidal volume |
| VDalv/VT | Ratio of alveolar dead space and tidal volume |
| VDalv/VTalv | Relationship of alveolar dead space and alveolar tidal volume |
